10
Oct
2024
If you are a doctor, nurse or aesthetic practitioner and you have just started injecting leg spider veins by Microsclerotherapy, you know just how frequently brown marks and staining occur after a session of Microsclerotherapy.
Incidence
In the medical literature, the published reported short-term incidence of pigmentation ranges from 10% to 30%. Post-sclerotherapy pigmentation is usually due to a combination of both melanin and haemosiderin pigment deposits. Melanin is formed as part of the natural healing process after Microsclerotherapy. It’s part of the post-inflammatory pigmentation process and hemosiderinis derived from extravasated red blood cells. Extravasated red cells are those that have left the blood vessel, entered the interstitium and deposited iron into the tissues.
In my opinion, I think the reported incidence is much lower than it actually occurs. I think some degree of pigmentation after sclerotherapy occurs in all cases if you look closely enough, so what we are REALLY talking about here in this article is excessive hyperpigmentation. This is the sort that goes on for 12 months that causes distress to your patients. So what can you do about this?

Causes of Excessive Hyperpigmentation
I'm going to cover the 4 major reasons why excessive hyperpigmentation develops after Microsclerotherapy and I’m going to tell you what you can do about it. And if you read until the end, I will share with you my top tip for dealing with established brown marks - marks that persist beyond 12 months - so that you can avoid complaints from your patients.
The first reason is that the sclerosant used was too strong. This is the usual and most common reason. For leg spider veins and blue reticular veins, I advise liquid Polidocanol - also called Aethoxysklerol - at 0.5% or you can use liquid STD (Fibrovein) at 0.2% . I suggest that you stick with liquid and that you avoid the use of foam sclerotherapy. Foam is much stronger, even at the same concentration. If hyperpigmentation continues to be a problem in your practice, consider diluting down to 0.25% Polidocanol or 0.1% STD.
The second reason is the presence of persistent reflux in associated reticular veins, a small perforator vein or even reflux in adjacent varicose veins. So if you think this might be a problem, re-examine the area under the brown marks and staining with a transillumination device such as Veinlite and check for varicose veins with your patient in the standing position. You might want to check for persistent reflux in and around the brown marks with high frequency ultrasound. Finding a small perforator vein or a reticular vein can be difficult, even with high frequency ultrasound, so if you think that might be a problem, consider referral to a more experienced colleague if you think that might be helpful and appropriate.
The third reason is that there is major reflux in a major truncal vein such as the saphenous vein - the great saphenous vein or the small saphenous vein. This can be an issue particularly if spider veins are clustered around the ankle, even in the absence of varicose veins. The condition is called Corona Phlebectatica. You should consider examining or re-examining the patient - particularly if spider veins and brown marks are around the ankle - by a complete venous duplex ultrasound.
The fourth reason is that there has been excessive thrombus formation after the Microsclerotherapy injection session. All sclerosants work by removing the delicate lining of the vein - the endothelium - and they initiate a local thrombus formation: clot within the vessel. If this clot formation is excessive, the presence of the clot stimulates continued inflammation and this inflammation will cause hyperpigmentation. The clot will eventually extravasate through the vessel and deposit iron into the tissues.

In some cases excessive thrombus formation can be reduced by applying a compression bandage immediately afterwards and you can also reduce the amount of thrombus after sclerotherapy by asking your patient to wear - compression stockings.
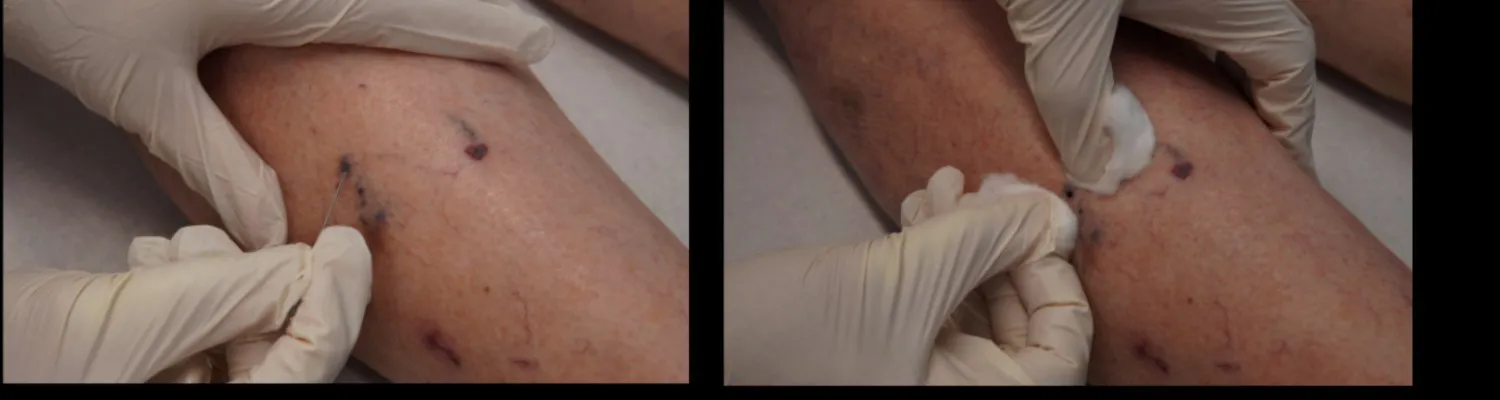
In addition, many specialists - myself included - recommend that you see patients 2 weeks after Microsclerotherapy and if there is any thrombus present - which will be obvious because the area will be hard and tender - you can prick these areas with a needle using an aseptic technique and release the thrombus. This is callled "Thrombectomy".
So there you are, those are the 4 major reasons why you may encounter excessive hyperpigmentation and I have explained what you can do about it.
Phototherapy to Avoid Complaints
At the beginning of this article, I told you I was also going to give you my top tip for reducing complaints in those patients who have established hyperpigmentation. I call it, perhaps a little flippantly, phototherapy. It’s not what you might think: It consists of developing a routine of taking photographs before treatment, immediately afterwards, and at all follow up appointments. In this way you can establish what has happened; how much pigmentation there is. If a patient is unhappy with the brown marks, you can offer to see them regularly and review photographs with them sympathetically. You may need to see them every 6 months for 2 -3 years because it really can take that long for hyperpigmentation that has been fully established to fade . Of course, you need to go through the other bits that I have discussed. You need to re-examine them, you need to check for persistent reflux and so on.

Brown Marks After Sclerotherapy Are Very Common. The main strategies to avoid hyperpigmentation are:
Avoid Excessively Strong Sclerosants
Treat Reticular Veins
Suspect and Treat Truncal Reflux
Evacuate Thrombus Formation
Serial Photography is a way of reassuring your patients that the hyperpigmentation is fading.
If you have made it to the end of this article, thank you! If you have any questions or comments, do please get in touch. I always like to hear from my readers. Your messages and comments comes straight into my own email inbox and I read them all personally.