
18
Nov
2010
Some of you may have seen Amanda Platell's article in the Daily Mail about Photodynamic Therapy (PDT for short) and the treatment of skin cancers and skin pre-cancers.
In essence, the article described the use of chemicals applied to the skin which then make rapidly growing skin cancer cells very susceptible to the damaging effects of particular light sources.
Normal surrounding skin cells are unaffected so collateral damage is very limited. The technique can be used for other tumours in which case the photo-sensitising chemical is either swallowed or injected.
This technique does not involve the use of radiation - it just relies on the increased susceptibility of rapidly growing (jargon = hyperproliferative) skin cancer cells to take up the sensitising chemical and then become much more vulnerable to light.
The British Association of Dermatologists has produced a very good patient information leaflet on PhotoDynamic Therapy and also on Basal Cell Carcinomas.
The disadvantage of photodynamic therapy is primarily that it can only be used for certain types of skin cancer and pre-cancers and these have to be carefull assessed and pre-determined by taking a very fine biopsy sample for laboratory analysis.
The treatable skin cancers are basal cell carcinomas, Bowen's Disease and also actinic keratosis. Anatomical positioning is also important because although collateral damage to normal skin cells is most unlikely and unusual great care has to be used in areas such as the surrounds of the eye.
Malignant melanomas are currently definitely not amenable to treatment with routine photodynamic therapy or PDT at the moment.
What happens when using photodynamic therapy?
Well to begin, a skin biopsy, usually using a device called a punch biopsy is taken to make the diagnosis. This sounds rather horrid but there is no "punching" involved. Following application of a small amount of anaesthetic a tiny 2mm core of tissue is taken from the suspect target skin cancer.

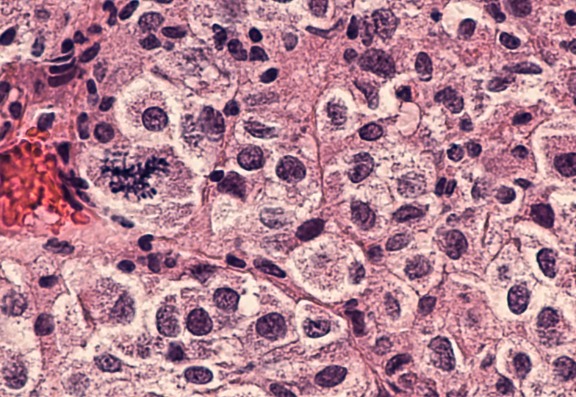
The sample is sent for histology at a laboratory where the exact type of skin cancer or pre-cancer is determined and also very importantly the depth of the tumour.
The depth is important because there are some sorts of basal cell skin cancers which do not respond to photodynamic therapy because they are too deep. These need to be surgically removed.
How does PDT - photodynamic therapy, work?
A specially prepared chemical cream called methyl aminolevulinate (MAL) is applied to the target area and then covered with a dressing which keeps out light. This remains on the skin for a variable period - usually, a few hours and the patient is free to leave the clinic and return later.
The MAL will cause the production of porphyrins in the rapidly growing and dividing cancer cells. By exposing the target area which had previously been covered by the MAL cream to a specific red or blue wavelength light, the porphyrins will create oxygen-free radicals within the cells which will then kill the cancer cells.
Typically two treatments are needed at a 7-day interval. During the application of the cream and also the application of the red or blue light source there is usually no pain.
After the light exposure has finished there can be quite an intense discomfort localised to the target area which a few patients have likened to a hot "fizzing" sensation. This is generally anticipated and controlled by painkillers ahead of the use of the light treatment.
So in summary, the skin cancer is confirmed and identified by the biopsy specimen; the patient returns when the histology result is available; the first application of the cream is used and then three or so hours later the red or blue light is applied for a few minutes. The patient is then free to go home and rest and to return in 7 days for the second treatment.
Ongoing surveillance does need to be carried out over a lifetime. Patients with basal cell carcinoma tend to be either genetically susceptible e.g., with Celtic skin colouring and to have been heavily sun-exposed and so usually the first basal cell carcinoma is just that - the first, and others can be expected.
The very definite advantage for basal cell cancers, Bowen's Disease or actinic keratoses which fall into this treatment category is that the treatment avoids fairly substantial surgery. With Amanda Platell's skin cancer, she had a big surgical excision over her eyebrow with a recurrence of cancer some years later at the same site. Standard surgical treatment the second time around would likely have resulted in her eyebrow being removed as part of the surgery. This would not be a desirable outcome for anyone.
Hey, wait!
Before you go.....
Let's stay in touch, pop your details here and we'll send our editor's hand-picked updates on your fave subjects.